Overview of Arthritis and Selected Types of Arthritis
Arthritis means inflammation of a joint, usually accompanied by pain, swelling, and changes in structure. Rheumatism is a general term for acute and chronic conditions characterized by inflammation, muscle soreness and stiffness, and pain in joints and associated structures, including arthritis (infectious, rheumatoid, gouty), arthritis due to rheumatic fever or trauma, degenerative joint disease, neurogenic arthropathy, hydroarthrosis, myositis, bursitis, fibromyositis and many other conditions.6
The Arthritis Foundation defines arthritis as encompassing more than 100 diseases and conditions affecting joints, the surrounding tissues, and other connective tissues, including osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus, juvenile rheumatoid arthritis, gout, fibromyalgia, bursitis, rheumatic fever, and Lyme disease. The three most common forms of arthritis are osteoarthritis, rheumatoid arthritis, and fibromyalgia.7 Approximately 21 million Americans are estimated to have osteoarthritis, approximately 4 million are estimated to have fibromyalgia, and approximately 2 million are estimated to have rheumatoid arthritis.1
Additional common conditions of arthritis symptoms include gout and bursitis/tendonitis. Other numerous uncommon conditions collectively make up most of the remaining prevalence.
In 1995, the NADW identified the ICD-9-CM diagnostic codes for all potential conditions of arthritis and rheumatism. From the individual codes, 39 groups and selected individual codes were formed. To assist in studies, 10 categories were developed from the groups and individual codes.8,9 A brief overview of four of the more common specific types of arthritis follows. Prevention, causation, treatment, and acuity or chronicity may vary significantly depending upon the specific condition under consideration.
Osteoarthritis
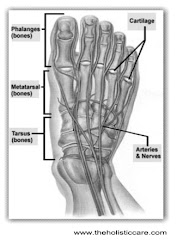
Osteoarthritis (OA) is the most common form of arthritis . It may be defined as a heterogeneous group of conditions that lead to joint symptoms and signs that are associated with defective integrity of the joint cartilage, in addition to related changes in the underlying bone and at joint margins.10 Radiologic evidence of OA is present almost universally in at least one joint after the age of 75.11 Yet, in population studies, only 40% to 80% of those with radiologic OA have joint symptoms. Subjects with more severe x-ray findings have higher rates of symptoms.12 The joints most commonly affected are those of the hand, lumbosacral and cervical spine, hip, knee, and foot.
Estimating the prevalence of OA is problematic. Objective diagnosis of OA is based on radiographic findings. The radiographs must show the presence of osteophytes, or bony outgrowths.13 This implies that the prevalence of OA should be reported for specific joints. In addition, the decision to include mild as well as moderate or severe changes will affect prevalence estimates.1
The strongest known risk factors for OA are older age and female sex. Osteoarthritis rates are similar in men and women under age 45, but after age 50, women in all populations have a higher prevalence than men, with more joints involved and more symptoms.14 Obesity and overweight have demonstrated a positive relationship with OA of the knee and possibly OA of the hip and hand.15 Socioeconomic factors associated with OA include having less than high school education and having a low family income.16 The comparative role of biological, lifestyle, and socioeconomic factors in ethnic differences in osteoarthritis is uncertain. Additionally, the role of genetics is strong in determining who will get osteoarthritis.17
Occupations requiring repetitive trauma to joints may have an effect on later development of OA in those joints.11 Continuous overuse of a particular joint may also influence later development of OA.18 Acute major joint injuries common during sports activities frequently lead to OA. This may explain the high rate of OA of the knee in retired professional athletes. The association between leisure time sports and OA is not clear, although acute major joint injuries rather than repeated joint use may account for the higher rates of OA seen among sports enthusiasts.14
Osteoarthritis leads to pain, stiffness, mobility problems, and activity limitations. Prevention measures include preventing obesity and joint injury, and use of ergonomics in the workplace.
Treatment measures are typically comprised of medications for pain, physical therapy, surgery (hip and knee replacement and other surgical procedures) and programs for self-management, exercise, weight loss and nutrition.19
Rheumatoid Arthritis
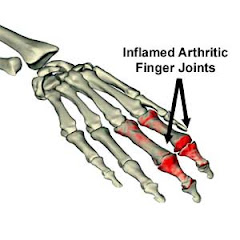
Rheumatoid arthritis (RA) is a chronic, inflammatory, systemic disease affecting the lining of the joints. The usual symptoms are pain, stiffness, and swelling of multiple joints. It commonly affects the small joints of the hands and wrists leading to nodules and deformities. It affects other joints as well and can affect the connective tissue throughout the body, as well as such organs as the lungs, heart, and eyes.20
Peak incidence of RA occurs between the fourth and sixth decade of life. Other known risk factors include genetic predisposition, hormonal factors, and a positive test for rheumatoid factor. The disease occurs two to three times more frequently in females than males. It has a worldwide distribution and affects all ethnic groups.21 A protective relationship between the use of oral contraceptives and RA was indicated in some studies22,23 although not found in others.24,25
Primary prevention of RA is not possible, as the cause is unknown, although attempts have been made to find an infectious agent. However, since most joint destruction occurs early in the disease, prompt diagnosis and treatment may help prevent the irreversible joint damage. The median lag time between the onset of symptoms and diagnosis is 36 weeks, with a range from 4 weeks to more than 10 years.26 Treatment embraces the use of medications, occupational and physical therapy, surgery, and self-management programs.
Life span may be shortened by 3 to 18 years in those with more severe disease and comorbidities. This is due to infections, gastrointestinal complications of therapy, and pulmonary and renal disease.27 One important area for tertiary prevention in connection with this disease stems from the excess mortality from respiratory and infectious diseases. This underscores the need for a major public health effort with respect to immunization with pneumococcal and influenza vaccine.28
Encouraging news is that the incidence of RA may be declining29,30,31 although some studies have not shown a decline.32,33 Also, the severity of the disease may be decreasing.33,34 These changes may be due to a change in a causative infectious agent, increased use of oral contraceptives, early initiation of treatment, or improved socioeconomic conditions.14 Theroleof oral contraceptives in particular is highly uncertain, due to the wide discrepancy in results among studies.35
Juvenile rheumatoid arthritis (JRA) is the most common form of childhood arthritis, affecting about the same number of children as juvenile diabetes.36 Onset is usually at less than 16 years of age. Up to half of those with JRA diagnosed as children may no longer have symptoms as adults. However, up to 30% of JRA patients may have significant functional limitations after 10 or more years of follow-up. In addition, mortality rate estimates for individuals with JRA range from 3 to 14 times greater than the rate for a similarly aged US population.37
The most commonly cited prevalence estimate is of 70,000 to 100,000 active and inactive cases of JRA in the United States under age 16.38 An estimate of the number of people over age 16 with active JRA in the United States is 35,000 to 50,000.39
Fibromyalgia Fibromyalgia is the most common rheumatic cause of chronic diffuse pain. It is defined as a syndrome involving pain and multiple tender points throughout the body, sleep disorders, irritable bowel syndrome, and headaches. It has predominance in females (more than 75%), and a peak incidence among persons 20-60 years of age. Factors associated with fibromyalgia include a history of major depression40 and or trauma, migraine, irritable bowel syndrome, sleep disturbances and sleep apnea.41 It has been observed among 15% of rheumatology patients and in 5% of patients in a general medical practice.42 Prevalence was 2% in a random sample of midwestern residents43, which is also in agreement with the NADW estimates.
this information was provides by Consultora en Finanzas Net Managing
domingo, 19 de agosto de 2007
Arthritis Symptoms - Gout - Osteoarthritis
Publicado por
SEO Consultant
en
11:12
![]()